Long QT Syndrome (LQTS)
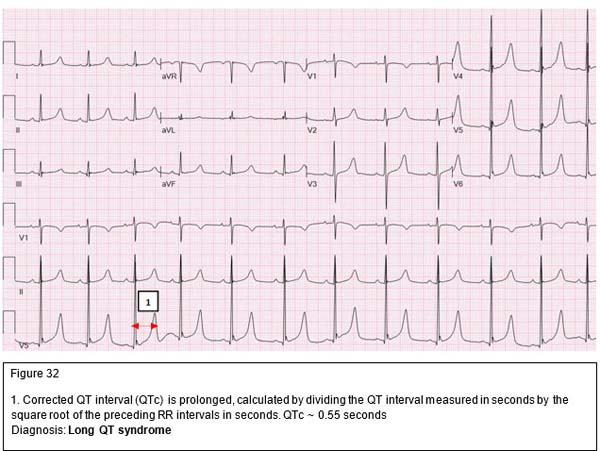
The QT interval represents both ventricular depolarization and repolarization. The QT interval varies with heart rate. The faster the heart rate, the shorter the QT interval. The corrected QT (QTc) interval is calculated by dividing the measured QT in seconds by the square root of the preceding R-R interval in seconds. A corrected QT greater than 0.46 seconds is considered prolonged. In normal neonates, the QTc may be 0.50 seconds in the first few days of life.
LQTS is an inherited condition characterized by syncope, seizures, palpitations or even sudden death. There are four different classes of patients with LQTS:
- Jervell and Lange-Nielsen syndrome, which is inherited in an autosomal recessive fashion and is commonly associated with sensorineural deafness
- Romano-Ward syndrome, which is inherited in an autosomal dominant fashion and is not associated with deafness
- The QT interval may be prolonged beyond the neonatal period by certain drugs (Table 2), toxins and electrolyte imbalance
- Sporadic cases of LQTS have also been reported
|
Antipsychotics |
Antiarrhythmics |
Tricyclics |
Other antidepressants |
Antihistamines |
Others |
|---|---|---|---|---|---|
|
Chlorpromazine |
Quinidine |
Amitriptyline |
Citalopram |
Diphenhydramine |
Erythromycin |
|
Haloperidol |
Procainamide |
Doxepin |
Escitalopram |
Loratadine |
Clarithromycin |
|
Droperidol |
Disopyramide |
Imipramine |
Venlafaxine |
Terfenadine |
Quinine |
|
Quetiapine |
Flecainide |
Desipramine |
Bupropion |
|
Chloroquine |
|
Olanzapine |
Sotalol |
|
|
|
Hydroxychloroquine |
|
Thioridazine |
Amiodarone |
|
|
|
|
Table 2: Common drugs which may cause QT prolongation
Pathophysiology
Congenital long QT syndrome may be caused by an imbalance of the sympathetic innervation in the heart especially the stellate ganglion or derangements in the cardiac ion flow, resulting in prolongation of the action potential. During the latter phase of the action potential, the myocardium is very excitable and may develop arrhythmia if stimulated electrically or mechanically. If a PVC occurs during this phase of the action potential (R on T phenomenon), a delayed after-depolarization develops in the form of a specific polymorphic ventricular arrhythmia (Torsades de pointes).
No discernable P waves, wide QRS complexes twisting around isoelectric axis
Dianosis: Torsades de pointes
Clinical
Most patients are asymptomatic. Symptomatic patients present with episodic dizziness, palpitations, syncope, seizures, and/or cardiac arrest. Patients with long QT syndrome can develop Torsades de pointes, bradyarrhythmias, or AV block. This can be triggered by exercise, emotions or loud noises.
Making the Diagnosis
- Clinical history.
- Family history of arrhythmia or sudden cardiac death.
- QTc> 0.46 second (beyond the neonatal period), bradycardia, second degree AVB, multiform PVCs and T wave changes (T wave alternans, bifid T wave or biphasic T wave).
- Further testing: Holter or event monitors, stress test and other electrophysiologic studies.
Management
LQTS is a serious condition. The risk factors for sudden death include long QT > 0.55 seconds, family history of sudden death, bradycardia for age, and a prior history of symptoms. Any medications that may cause QT prolongation should be discontinued.
Treatment is aimed at preventing conversion to other possibly fatal arrhythmias. Beta-blockers are the mainstays of medical management. An implanted cardioverter-defibrillator (ICD) is often used as a nonpharmacological treatment. Other treatment modalities include permanent dual chamber pacemaker and left cardiac sympathetic denervation.

