The Cardiac Cycle
|
|
|
||||||||
|
Cardiac cycle of the left side of the heart. The electrocardiogram (EKG) below the diagram shows the corresponding waves with each phase of the cardiac cycle. The bottom line represents the first and second heart sounds. |
|||||||||
The cardiac cycle represents the hemodynamic and electric changes that occur in systole and diastole. It has many phases.
Phases of the Cardiac Cycle
- Isovolumetric ventricular contraction (a-b): This phase marks the beginning of systole and starts with the appearance of the QRS complex on the EKG and the closure of the AV valves at point (a). With all valves closed, the ventricle generates positive pressure without any change in its volume (isovolumetric) to overcome the semilunar valves resistance that open at point (b). This phase usually lasts for 6% of the cardiac cycle.
- Rapid ejection (b-c): As the semilunar valves open at point (b), there is a rapid ejection of blood due to increased ventricular contractility. The arterial pressure increases until reaching its maximum at point (c). This phase usually lasts for 13% of the cardiac cycle.
- Reduced ejection (c-d): This phase marks the beginning of ventricular repolarization as depicted by the onset of the T wave on the EKG. Repolarization leads to a rapid decline in ventricular pressures and hence the reduced rate of ejection. However, some forward flow of blood continues secondary to remnant kinetic energy from the previous phase. This phase usually lasts for 15% of the cardiac cycle.
- Isovolumetric relaxation (d-e): When the ventricular pressures drop below the diastolic aortic and pulmonary pressures (80 mmHg and 10 mmHg respectively), the aortic and pulmonary valves close producing the second heart sound (point d). This marks the beginning of diastole. The ventricles generate negative pressure without changing their volume (isovolumetric) so that the ventricular pressure becomes lower than the atrial pressure. This phase usually lasts for 8% of the cardiac cycle.
- Ventricular filling (e-a): As the AV valves open at point (e), ventricular filling starts. The initial rapid filling is mainly augmented by ventricular suction which results from ventricular untwisting and the return of each ventricular muscle fiber to its slack length. The ventricular pressure gradually increases until it equals the atrial pressure and the AV valves close (point a). This phase usually lasts for 44% of the cardiac cycle.
- Atrial contraction: Finally, near the end of ventricular diastole, the atrial contraction contributes about 10% of the ventricular filling volume. This is represented by the P wave on the EKG of the following cycle. This phase usually lasts for 14% of the cardiac cycle.
Heart Sounds
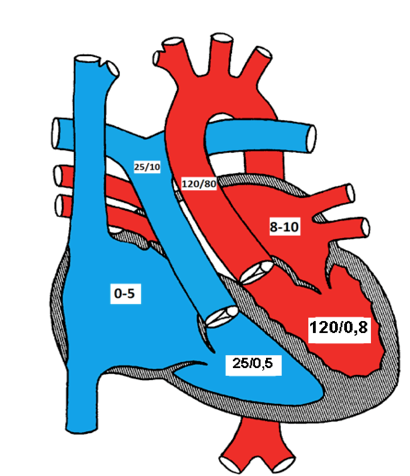
Normal pressures in various chambers of the heart
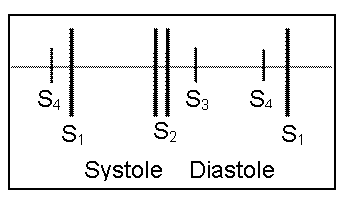
The first heart sound (S1) represents closure of the atrioventricular (mitral and tricuspid) valves as the ventricular pressures exceed atrial pressures at the beginning of systole (point a). S1 is normally a single sound because mitral and tricuspid valve closure occurs almost simultaneously. Clinically, S1 corresponds to the pulse.
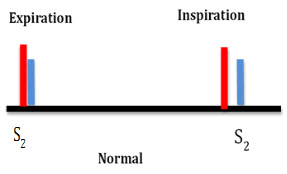
The second heart sound (S2) represents closure of the semilunar (aortic and pulmonary) valves (point d). S2 is normally split because the aortic valve (A2) closes before the pulmonary valve (P2). The closing pressure (the diastolic arterial pressure) on the left is 80 mmHg as compared to only 10 mmHg on the right. This higher closing pressure leads to earlier closure of the aortic valve. In addition, the more muscular and stiff "less compliant" left ventricle (LV) empties earlier than the right ventricle. The venous return to the right ventricle (RV) increases during inspiration due to negative intrathoracic pressure and P2 is even more delayed, so it is normal for the split of the second heart sound to widen during inspiration and to narrow during expiration. Clinically, this is more remarkable with slow heart rates.
The third heart sound (S3) represents a transition from rapid to slow ventricular filling in early diastole. S3 may be heard in normal children.
The fourth heart sound (S4) is an abnormal late diastolic sound caused by forcible atrial contraction in the presence of decreased ventricular compliance.
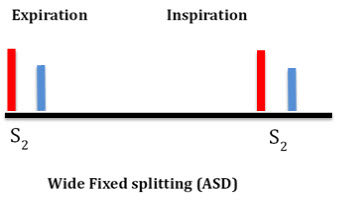
Abnormally wide splitting of S2 may occur in:
a) RV volume overload, such as atrial septal defect (ASD) and anomalous pulmonary venous connection. In these cases, the split is usually wide and "fixed" with no difference between inspiration and expiration due to fixed RV volume (see ASD section)
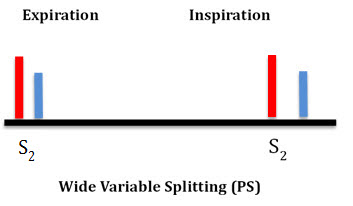
b) RV outflow obstruction, such as pulmonary stenosis (PS)
c) Delayed RV depolarization such as complete right bundle branch block
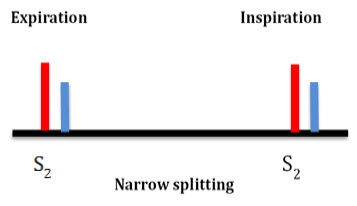
Narrow splitting of S2 occurs in:
a) Pulmonary hypertension as the pulmonary valve closes earlier due to high pulmonary resistance
b) Mild to moderate aortic stenosis as the A2 is delayed
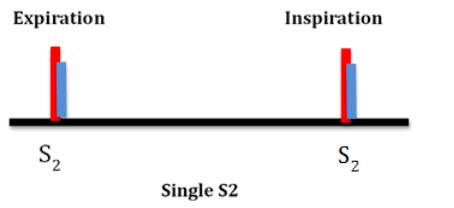
Single S2 may occur:
a) If one of the semilunar valves is missing, as in pulmonary or aortic valve atresia and truncus arteriosus
b) If both valves close simultaneously as in pulmonary hypertension with equal pulmonary and aortic arterial pressures
c) If both valves close simultaneously as in double outlet single ventricle or in large VSD with equal ventricular pressures
d) Posterior displacement of the pulmonary valve away from the chest wall as in d-TGA
Paradoxical splitting of S2 (P2 is heard before A2) occurs in:
a) Severe aortic stenosis
b) Left bundle branch block
In both conditions, the aortic valve (A2) closes after the pulmonary valve (P2). Since the respiration only affects P2, its effect in paradoxical splitting is the opposite of normal, i.e. inspiration causes narrow splitting while expiration causes wide splitting of S2.
Heart Murmurs
Murmurs are additional sounds generated by turbulent blood flow in the heart and blood vessels. Murmurs may be systolic, diastolic or continuous.
Grading of systolic mumers based on thier intensity
- I/VI: Barely audible
- II/VI: Faint but easily audible
- III/VI: Loud murmur without a palpable thrill
- IV/VI: Loud murmur with a palpable thrill
- V/VI: Very loud murmur heard with stethoscope lightly on chest
- VI/VI: Very loud murmur that can be heard without a stethoscope
Systolic murmurs are the most common types of murmurs in children and based on their timing within systole, they are classified into:
a) Systolic ejection murmurs (SEM, crescendo-decrescendo) result from turbulent blood flow due to obstruction (actual or relative) across the semilunar valves, outflow tracts or arteries. The murmur is heard shortly after S1 (pulse). The intensity of the murmur increases as more blood flows across an obstruction and then decreases (crescendo-decrescendo or diamond shaped). Innocent murmurs are the most common cause of SEM (see below). Other causes include stenotic lesions (aortic and pulmonary stenosis, coarctation of the aorta, Tetralogy of Fallot (TOF)) or relative pulmonary stenosis due to increased flow from an ASD
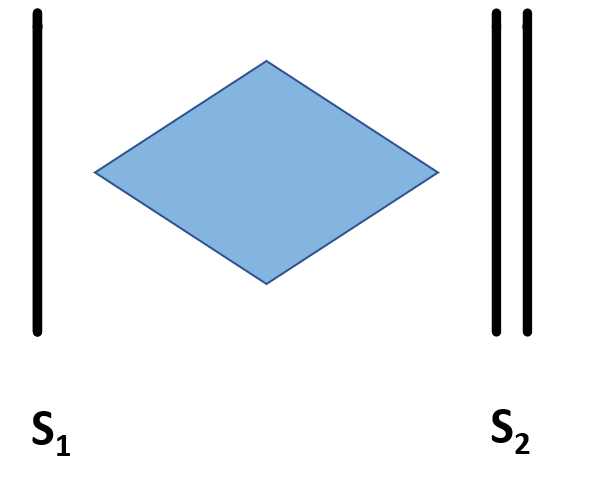
Crescendo decrescendo murmur
b) Holosystolic (regurgitant) murmurs start at the beginning of S1 (pulse) and continue to S2. Examples: ventricular septal defect (VSD), mitral and tricuspid valve regurgitation.

Holosystolic murmur
c) Decrescendo systolic murmur is a subtype of holosystolic murmur that may be heard in patients with small VSDs. In the latter part of systole, the small VSD may close or become so small to not allow discernible flow through and the murmur is no longer audible.
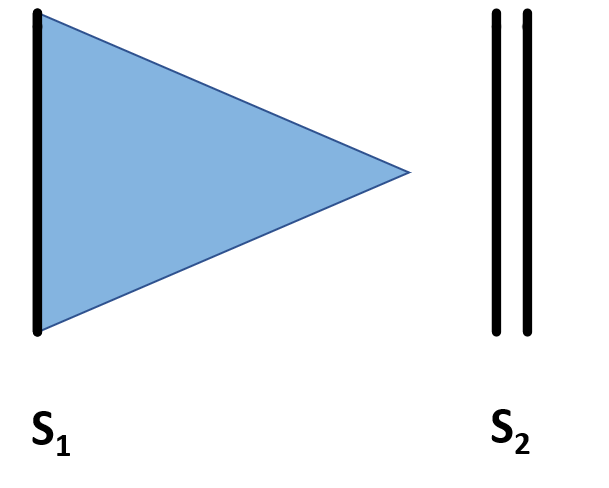
Decrescendo murmur
Diastolic murmurs are usually abnormal, and may be early, mid or late diastolic.
More information: Examples of innocent murmurs
- Early diastolic murmurs immediately follow S2. Examples: aortic and pulmonary regurgitation.
- Mid-diastolic murmurs (rumble) are due to increased flow (relative stenosis) through the mitral (VSD) or the tricuspid valves (ASD).
- Late diastolic murmurs are due to pathological narrowing of the atrioventricular (AV) valves. Example: rheumatic mitral stenosis. Tricuspid stenosis is very rare in children.
Continuous murmurs are heard during both systole and diastole. They occur when there is a constant shunt between a high and low pressure blood vessel. Examples: patent ductus arteriosus (PDA) and systemic arterio-venous fistulas. This may also occur in surgically placed shunts such as a Blalock-Tauussig (BT) shunt between the aorta and the pulmonary artery.
Innocent murmurs are common in children and have the following characteristics:
- Grade III or less in intensity
- An otherwise a normal cardiac examination and normal heart sounds
- No associated cardiac symptoms
- Change in intensity with body position (e.g. louder in supine position)
Summary of Heart Murmurs
| Table showing the common systolic, diastolic and continuous heart murmurs | |
|
Systolic |
|
|
Diastolic |
|
|
Continuous |
|
| *Obstructive lesions include AS, PS, Coarctation of the aorta, TOF, etc. | |
| Table showing the common heart murmurs audible at different age | |
|
Immediately after birth |
PDA or obstructive lesions* |
|
Shortly after birth (a few hours to few weeks) |
VSD, PDA, PPS (peripheral pulmonary stenosis) |
|
1-4 years |
Innocent murmurs, ASD |
|
Teenage |
Innocent murmur, HOCM or MVP/MR |
| *Obstructive lesions include AS, PS, Coarctation of the aorta, TOF, etc | |